Survivor Stories Blog
Drug Diversion Support Groups: Hope for Addicted Nurses

Today I would like to share a bit about the Florida Board of Nursing’s “Intervention Project for Nurses” or IPN. It is similar to other Drug Diversion Programs that many states have, but it has a piece to it that is a bit different…they have a statewide support groups for nurses. This interests me, what a great idea. To have nurses that have been through the same issues regarding drug diversion talk to those who are beginning their journey is a very valuable tool.
“The mission of IPN is to ensure public health and safety by providing an avenue for swift intervention/close monitoring and advocacy of nurses whose practice may be impaired due to the use, misuse, or abuse of alcohol or drugs, or a mental and/or physical condition. IPN is authorized by Florida Statute, Chapter 464/456, to assist those nurses whose practice is affected.”
“Program Objectives…
- To ensure public health and safety through a program that provides close monitoring of nurses who are unsafe to practice, due to the use of drugs including alcohol and/or psychiatric, psychological or a physical condition (chapter 455.261).
- To provide a program for affected nurses to be rehabilitated in a therapeutic, non-punitive, and confidential process.
- To provide an opportunity for retention of nurses within the nursing profession
- To facilitate early intervention, thereby decreasing the time between the nurse’s acknowledgment of the problem and his/her entry into a recovery program.
- To require the nurse to withdraw from practice immediately, and until such time that the IPN is assured that he/she is able to safely return to the practice of nursing.
- To provide a cost effective alternative to the traditional disciplinary process.
- To develop a statewide resource network for referring nurses to appropriate services.
- To provide confidential consultations for Nurse Managers.”
The IPN has a vast network of resources for nurses. Florida has 150 Nurse Support Groups throughout the state. Each group has a facilitator. This is what one had to say, “I have been a Nurse Support Group Facilitator for over 12 years. I have witnessed many nurses come and go from my groups. The “magic” of the Nurse Support Group lies in the fact that a nurse who feels totally alone and full of negative self-talk and shame, secondary to his or her substance use disorder, attends group with other colleagues who have struggled with similar feelings and circumstances. There is a realization that “I am not alone anymore” and hope is born.” And one of the participants shared this, “Walking into my Nurse Support Group the first time surprised me. I will never forget the experience. My first surprise was how welcoming folks were to me. I listened as members shared a little about themselves with me, and I was amazed how similar the stories were to mine! I left that night with a sense of hope.”
I know when I first started this journey, I needed to speak to other people going through what I was. I was lucky in the sense that my counselor had another nurse she was treating with almost the exact same issues. What I didn’t have was someone who had been successful in going through the BON’s program and returning to practice. It would have been very helpful to have someone walk me through the process. As it was, I fumbled around with a lot of anxiety and some missteps. I would love to be a resource for nurses new to the BON monitoring program and new to sobriety. 12 step programs are essential in my opinion and they have worked so well for me, but they do not include anything about how to recover as a nurse. Including how to navigate the overwhelming program requirements, how to deal with the feelings of shame and remorse, how to get to a point where working as a nurse is a possibility again. I could be that resource, there are many like me that could. Together we can make a difference.
Eliminating Viral Hepatitis

“Ev, you have Hepatitis C. The lab test is postive, but I have no idea how you got it.”
My husband Tom said these words to me on February 8, 2002. And thus began my life with Hepatitis C.
Months later we learned that I contracted Hepatitis C through reuse of syringes during chemotherapy. The oncology nurse drew blood from my port, put the blood in lab collection vials and then used the same syringe to access a large saline bag. That same saline bag had been contaminated with a Hepatitis C+ patient’s blood during his port flush. In all, 99 people who were engaged in the fight of their lives to overcome cancer were infected with this second deadly disease.
I’ve learned alot about Hepatitis C since then. Around the world 400 million people are infected with hepatitis B and C, more than 10 times the number of people living with HIV. An estimated 1.45 million people died of the disease in 2013 – up from less than a million in 1990.
Recently we celebrated World Hepatitis Day. It is a day to remember those who have died from the disease, support those who currently have it, and work towards prevention. The theme for this year is “Elimination.” The World Health Organization announced a strategy for dealing with the world-wide epidemic of viral hepatitis.
This new WHO strategy introduces the first-ever global targets for the elimination of Hepatitis B and Hepatitis C as public health threats. These targets include a 30% reduction in new cases of hepatitis B and hepatitis C, and a 10% reduction in mortality by 2020, and ultimately achieving even greater health impact by 2030. Key approaches to achieving these targets include:
- expanding vaccination programs for hepatitis B;
- preventing mother-to-child transmission of hepatitis B;
- improving injection, blood, and surgical safety;
- providing harm reduction services for people who inject drugs; and
- increasing access to diagnosis and treatment for hepatitis B and hepatitis C.
These are lofty goals, but so necessary.
I am one of the lucky ones. After exhausting treatment, I have no detectable virus in my bloodstream. I am profoundly grateful. I choose to live my gratitude by advocating for safe injection practices so that no one else will hear the words, “You have Hepatitis C, but we have no idea how you got it.”
Think NoHep this World Hepatitis Day
Today is World Hepatitis Day and this year’s theme is “Elimination.” The World Health Organization (WHO) recently adopted the first ever Elimination Strategy for Viral Hepatitis that calls for “rigorous application of universal precautions for all invasive medical interventions and promotion of injection safety measures…”
World Hepatitis Day is a great way to raise awareness about injection safety. Here are six ways you and your organization can get involved!
1. Read and share Dr. John Ward’s blog, “Think NoHep this World Hepatitis Day.”
2. Check out CDC.gov’s World Hepatitis Day Feature.
3. Connect with the One & Only Campaign and the World Hepatitis Alliance on Facebook and Twitter using the official hashtags #NOhep and #WorldHepDay.
4. Join the #NOHep Thunderclap to amplify the message on social media.
5. Pledge your support for the World Hepatitis Day campaign by sharing your organizations logo on the World Hepatitis Day webpage.
Announcing a new injection safety continuing education program

HONOREFORM’S LEARNING ACTIVITY PROGRAM
The Healthcare Learning Activitity Grant Program provides a quality continuing education presentation at low or no cost. HONOReform will provide a grant to organizations sponsoring

continuing education activities for healthcare professionals or consumer-focused activities.
Attendees will receive a flash drive containing the PowerPoint presentation, resources for injection safety, and the award-winning book: A Never Event: Exposing the Largest OUtbreak of Hepatitis C in American Healthcare History.
Description of Offered Programs
Healthcare providers in all types of settings have reviewed and followed safe injection best practices. Nonetheless, the “unthinkable” still happens, with significant impact on the patient and providers. The CDC estimates that there have been more than 50 outbreaks of Hepatitis C and/or Hepatitis B in the past decade due to reused needles, syringes or medication vials. Evelyn and Tom McKnight, founders of HONOReform, will share their own compelling story of infection attributed to reuse of syringes in a medical setting. Additionally, the McKnights will examine factors contributing to the outbreak and make recommendations for prevention.
1. “A Never Event – Don’t let it Happen in your Facility!”
A survivor describes a Nebraska “Never Event” in which 99 patients contracted Hepatitis C when a nurse reused syringes during chemotherapy administration. Root causes of the outbreak are examined as well as resources for prevention.
2. “Preventing Healthcare Transmission of Disease through injection Safety”
This presentation examines causes of patient-to-patient, patient-to-provider and provider-to-patient transmission of disease and offers resources for prevention.
3. “Injection Safety in Dental Practice”
Since 2012 thousands of patients have been put at significant risk of acquiring infectious disease from dental practices in four states. In one instance, the Colorado Department of Health notified 8000 patients that they were at risk for contracting Hepatitis B, Hepatitis C and HIV because their dentist’s practice reused needles and syringes. The McKnights will examine factors contributing to the outbreak and make recommendations for prevention in dental offices.
4. “Becoming an Empowered Patient”
Patients are learning that to receive the best quality healthcare, they need to effectively partner with their healthcare provider. A physician and a survivor of medical error discuss their own personal experiences of patient empowerment and ways to improve the physician-patient partnership.
For more information and to apply, go to Learning Activitiy Program
**********************************************************************************
It is my honor to highly recommend Dr. Evelyn V. McKnight as a speaker. I can think of no one better to present this information. Without a doubt, she exemplifies the motivation and goal-directed approach, in concert with the knowledge and passion to deliver this complex issue. Wanda O. Wilson, PHD MSN, CRNA, Executive Director, American Association of Nurse Anesthetists
Evelyn tells her story with compassion and purpose with the intention to educate listeners about the egregious unsafe practices that continue unabated in healthcare practice sites. I enthusiastically recommend Evelyn McKnight to any group seeking to educate and inspire its members! Janice M. O’Dowd, Certified Continuing Medical Education Professional, Kent Hospital, Warwick, Rhode Island
The McKnights put together an extensive slide show presentation, with multiple resources for further education. They provided tools for healthcare providers to use in their jobs to help educate other providers and present healthcare associated infections. … If you are looking for an engaging educational presentation for your next healthcare conference, I would recommend Tom and Evelyn McKnight. They were very well received, and did a wonderful job. Michele Maryanski, RN CIC, APIC New England Program Director
Our feedback following this course was absolutely outstanding! We hope that Evelyn will continue to educate the public and bring more awareness on safe injection practices so an event like this never happens again. Melissa Adams, Continuing Education Director, AZ Perio Dental Hygiene Study Club
Devastating Loss – a Blog by Kristin, RN

Kristin has been a Registered Nurse since 1991. After losing so much to alcohol and drug addiction, she turned her life around and has been sober for more than 11 years. Kristin now works in the clinical research industry, has published a book about her story of addiction and recovery, and works with others who face those same struggles. Her blog focuses on the reality and pervasiveness of the problem (especially in healthcare) and offers real solutions to those who are ready to hear them. She regularly posts a blog about drug diversion among healthcare providers. Her post from April 3, 2016 is shown here. You can also access Kristin’s blog here.
Last month I heard about a young nurse, age 23, who died of a heroin overdose. Jessica was dropped off at an ER in a comatose state by an unknown man. There were track marks on her body. Her family was stunned, they had no idea she used drugs. She was a nurse at a local hospital; she was studying to become a registered nurse. Her family said there were no signs that indicated she had a drug problem…no signs. That is the key point in this story to me. Nobody knew I was using either. We addicts can be so good at hiding our drug use. This is why we need to be randomly drug tested. Maybe if they had this requirement at the hospital where Jessica worked they would have caught her. Sure, it would have been devastating to this young nurse. Her career dreams would have been seriously altered. But she would have been alive. She would have had the opportunity to start her life, her career over again. She may have been successful at fighting her addiction, she may not have been, but she would have had a chance. She has no chance now. It is such a waste of a life, what could have been a beautiful life.
I used drugs for years and nobody knew – nobody. I was smart, or so I thought. I knew how much I could take while working so that nobody would suspect. Please note that I write ‘while working’. I did not just do this in the privacy of my home while my children were safely tucked in bed. No, I did it whenever I could. While working, while driving, while taking care of my kids, while visiting friends and family, anytime I had drugs to take. As my addiction progressed I became less able to control when and where I used them.
Yet I was one of the lucky ones, although it didn’t feel that way at the time. I got caught before having to suffer Jessica’s fate. Nobody suspected I was using until the stock supply started disappearing. You see, after a time I could no longer wait for the ‘waste’ drugs, I craved them so badly. Once I started taking the stock supply it didn’t take them long to figure out it was me. I was arrested and charged with 26 felonies. I was absolutely devastated. I had no idea what I was going to do. But again I say, I was one of the lucky ones; I ended up getting clean (after a few more stumbles) and have stayed that way for 11 years (and counting). I am a nurse in good standing again.
I think the most important thing to take away from this blog is that you can’t always tell if someone is using drugs or not using drugs. If you depend on being able to identify those with a substance abuse problem by sight you will be missing many of them. Sure there are some that reek of alcohol, pass out in bathrooms or get arrested, those are the obvious cases, but there are just as many that are hiding an addiction that nobody can see. They are the ones that we need to focus our attention on. They are the ones that may be helped if random urine drug screens would be required of all healthcare workers with access to controlled substances. Detecting their problem could prevent a death. The death of the addict or their patient’s death. They are dangerous, I was dangerous. I didn’t think so at the time, I thought I had it all figured out. But I was fooling myself. Anyone who is high at work is risking their patient’s safety. Their decisions and reactions are flawed.
Please join me in my quest to get people to listen. The public needs to understand the scope of the problem. The Licensing Boards need to advocate for random drug testing. The government needs to require it. I am one voice and few are listening to me. I need more voices.
Mentoring the next generation of physicians in patient safety
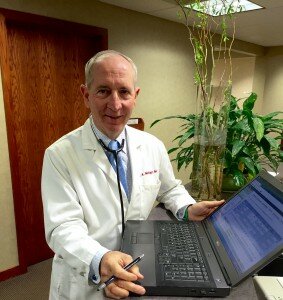
Dr Tom McKnight was recently awarded the University of Nebraska Medical Center’s Koefoot Award for outstanding teaching and mentoring of medical students during the family medicine rural preceptorship. Following are some excerpts from Dr McKnight’s acceptance speech.
Thank you, Koefoot family and the department of family medicine. I am humbled and honored by this award. I know that there are many deserving family physicians in our state that mentor students in outstanding, compassionate care on a daily basis. I read a quote by Gretchen about her father. She said, “Medicine was his life and his love. He devoted all of his time and energy to his practice in Broken Bow.” I hope my own sons will likewise admire the way I have conducted my practice.
I chose to go into family medicine because it provides the opportunity to be involved in peoples’ lives from birth to death. I’ve enjoyed the family medicine experience because of the broad range of challenges emotionally and intellectually whenever I step into an exam room. In my daily routine I often celebrate with new parents when they bring their baby to the doctor for the first time and then go to the next exam room to break the news to a married couple that the husband has terminal lung cancer and has only a few months to live. I have to say family medicine is as challenging and exciting now as it was 35 years ago when I started my practice. Sharing these challenges and rewards with students has made my day to day work life so much richer.
When I was first asked to mentor students early in my career, I quickly agreed. I remembered fondly the time I had spent in Lynch, NE with Dr Becker on my family practice rotation, and I was anxious to provide that stimulating experience for others. At the time that I first accepted students, I was hardly older than the students. I was 28 when I started my private practice. I think back on that now, and am glad I was too naive to realize the big responsibility that I was undertaking. My parents were both teachers, and I think because they made teaching look easy, I thought it would be easy for me, too. I quickly came to a deep appreciation for how challenging teaching is, and gained a deep appreciation for how my parents had shaped so many lives in profoundly productive ways.
Being involved with medical students throughout my career has been extremely rewarding. It is a source of continued stimulation and motivation for keeping up with the advancements of medicine. Sharing the joy with a student of their first delivery or the satisfaction of suturing their first laceration gives me a warm feeling. Its interesting to show them private practice medicine and what it is like to be involved in a community. I love following their educational and career advancement and then have them as specialty consultants. Many of the more than one hundred students I have mentored over my career have become my lifelong friends.
One big challenge to family physicians of my generation was the implementation of electronic medical records. Medical students have played a key role in my education about digital records and have made the transition seamless. Not only have they helped me learn how to keep digital records, they taught me how to access valid information on the web and how to fulfill ongoing family practice continuing education on the internet. And – they also showed me the best apps for Nebraska football stats!
My family has shared the experience of precepting students with me. Evelyn has been a gracious host to the many students who have joined our supper table and who have lived with us throughout their rotation. When our sons were young, I could see how they started thinking about medicine as a career through watching students, which is a different way of seeing medicine than in watching Dad. I was privileged to mentor all three sons during their medical education. It was marvelous to see their compassion and care of patients during their family medicine rotations. It gave them an understanding of what my career is. I’m honored that they have chosen medicine for their own career paths and that they, in turn, mentor students. It’s rewarding and sometimes humorous to talk to them about their own patients. I got a phone call from Curtis the psychiatrist recently, asking me how to treat constipation!
My staff takes great interest in the education of the students. This has become even more important in the era of digital medical records because the first few days of a rotation is spent with staff as the student learns our office based system. Staff gets attached to the students and is sad to see them go when they leave, but are delighted to see their progress as compassionate physicians. Staff often spends more time with patients than I do, which teaches the students the value of teamwork in patient care.
The patient doctor relationship is special. I am privileged to care for 4 generations of families. I am so humbled that they have placed their trust in me, many for 3 decades.
Our patients are always very interested in students. They want them to learn well; they want them to do well. They want them to become exceptional Nebraska family physicians. I see how disappointed the patients are when they come to the office expecting to see their favorite student, only to learn that she has moved on. Patients still ask me about students, years after they have graduated. This is especially true when the student was involved in a family crisis or a family joy such as a birth or a triumph over a serious disease.
You wouldn’t think that something as serious as teaching young people how to be good doctors would provide opportunities for laughter, but the truth is, something funny happens nearly every day. Here are some examples:
We’ve had students (more than one) put a cast on the wrong arm. Or put a blue cast on a little bitty girl dressed in pink who is sobbing. The student thinks she is crying because her arm hurts, but in actuality, she is crying because she wanted a pink cast!
Fremont Health Center is not a big place, but we had a student who could not remember where to park, even after being shown numerous times. In the last week of the rotation, the security guards were threatening to tow.
One time, after a student had completed his first pap smear, the staff member moved the provider’s stool out of the way. The student wasn’t aware that the stool had been moved, and plopped down on the floor!
I asked a student to put a UNA boot on a patient’s foot. When I came into the exam room, there was a blue shoe bootie on the injured foot!
I’m generally a patient man, but sometimes the time it takes some new students to do their first suture repair in interminable. I try to encourage the student to speed things up a bit without worrying the patient by making the comment “The fibroblasts are restless.” Not always does the student crack the code, and I often get a puzzled look from both the student and the patient.
I appreciate the cultural diversity that students bring to our practice. Last fall I had the pleasure of introducing a Chinese student to Nebraska football. Seeing the pageantry of the Red Sea in Memorial Stadium through someone else’s eyes made the experience so much richer for me.
I’ve enjoyed opportunities to serve in ways other than office medicine. I’ve shared with students about our service trips to third world countries, membership on nonprofit boards, medical staff offices and our own patient safety foundation HONOReform. I hope that all of my students will find service opportunities in their careers that have been as fulfilling to them as mine have been to me.
Our own experience with medical error and the work of HONOReform has made me a better doctor because I understand both the doctor and the patient side of the relationship. I’ve learned how to accept responsibility and do the right thing, even when that is a very difficult thing to do. I try to pass these lessons on to the students. From the first day of a rotation, the student hears our story, and throughout our time together, I try to model transparency and ethical behavior in every patient encounter. I want them to become less defensive, more compassionate, and more grateful for this wonderful career as the years go by.
For all of these many gratifying experiences, I thank the students who have spent precious months of their four years of medical school with me. I thank the department of Family Practice for their confidence in me. I thank the Koefoot family for recognizing and supporting rural family physicians in Nebraska. Our work is not done, and I am eager to continue to mentor the next generation of family physicians.
Drug Diversion Reporting…what more can be done

My sincere thanks to the Denver Post’s David Osher and Christopher Olinger for their in-depth piece on drug diversion, reporting and treatment on 4/24/2016.
http://www.denverpost.com/news/ci_29806013/drug-addicted-dangerous-and-licensed-operating-room
In this piece, spurred on by the maelstrom of events which surrounded the arrest of a surgical tech from Swedish Medical Center the previous month, Osher and Olinger point out the simple truth that hospitals do not all prescribe to the same standard of safety and precaution when a drug diversion occurs. It was made clear that simply not reporting a theft, leaves open the possibility of hiring of these drug diverting healthcare workers at other facilities and allow them to continue their diverting ways. These reporters did an extensive job in reviewing state health department, licensing board and police records. And the results were unbelievable.
Read more
A Survivor reacts to a new outbreak

Recently West Virginia health authorities announced that a cardiac clinic is at the center of an investigation of a potential outbreak of viral hepatitis through unsafe injection practices. Johnny Robertson of North Carolina is a survivor of a similar outbreak and is an active advocate of injection safety. We are grateful to Johnny for his leadership in patient advocacy. Following is his reaction to the outbreak.
In January 2008, I heard the words, “You have hepatitis C.” This diagnosis changed my life completely.
I contracted hepatitis C during a stress test at a cardiology clinic in North Carolina in 2007. Later, it was revealed that a medical technician administered saline solution to a patient who was infected with this life threatening disease, then reused the same syringe to re-enter the vial. This contaminated the vial of medication with the virus. Subsequent patients who received an injection from the saline solution vial were exposed to the virus. Five patients were infected with the virus, but many more were exposed and were urged by the state health department to be tested.
Several weeks ago, West Virginia’s Department of Health and Human Resources sent letters to 2,300 people potentially exposed to hepatitis B, hepatitis C and HIV through cardiac stress tests at Raleigh Heart Clinic in Beckley. From the recent article (“Hepatitis cases linked to Beckley clinic likely caused by human error,” March 29), we know that 12 patients have been infected with hepatitis C or hepatitis B.
This tragic news strikes an eerily similar tone.
In addition to the dozen patients who have been infected, my heart breaks for the patients who sit and wait and worry while results from blood tests come back. I offer them my deepest support.
Outbreaks like this one oftentimes affect entire communities. Families and friends and colleagues are affected. They take a toll on the human psyche, and they are complicated and costly.
The truth of the matter is this could have been prevented. It did not need to happen.
Generally, healthcare in the United States is very safe. But sometimes, unsafe practices are used—brought about by ignorance, desire to cut costs, or the demand to see more patients in a shorter amount of time.
But there are efforts to educate both healthcare providers and consumers about the absolute need for safe injections in all settings.
I work alongside colleagues at Hepatitis Outbreaks’ National Organization for Reform and North Carolina’s One & Only Campaign. I am proud to serve as a spokesman for this award-winning campaign. I tell my story to healthcare providers throughout the state to help reeducate and advocate for injection safety, urging them to use “One needle, one syringe, and only one time!”
Patients need to have a voice in healthcare. No one in the United States should be infected with hepatitis C while receiving healthcare. My hope is to support those who are going through this very difficult time and allow the conversation to begin about tighter safety protocols, in West Virginia and elsewhere. There is help out there for those who need it. I know because I was once in this same situation.
Johnny Robertson
Healthcare workers and addiction by Kristin Labott-Waite

With all the recent drug diversion incidents swirling around, we thought we would feature a guest blogger, Kristin Labott-Waite, to share opinions on healthcare workers and addiction. This is a re-print from her blog posted January 2, 2016.
As I sit here today with my good friend Butch and his daughter Paige, I am reminded that life is very short. Paige has melanoma in her brain and it has been progressing in recent weeks. We do not know what to expect next and that is the scariest thing. While I sit here I am contemplating why things happen the way they do. Why, after all the shit I pulled am I healthy and strong, and 22 year old Paige is so sick. Paige has a 16 month old daughter to take care of too. It isn’t fair. She is on all kinds of pain medication, fentanyl patches, Dilaudid, morphine, meds she needs to keep the headaches at bay. I know that she is using those meds because she needs them. While we sit here at the hospital I worry about people stealing the meds she so desperately needs. Read more
Drug Diversion Management; A Resource Guide

Over the past few months, the news has been riddled with stories of a surgical tech who diverted drugs in 4 states. He was finally caught in Colorado when a fellow employee finally turned him in. But the question remains, how did he go from a Navy court martial to wreaking havoc across multiple states and several hospitals?
We hear more about drug diversion, especially over the last decade, because we are catching more diverters. Kim New, executive director of the International Health Facility Diversion Association, states that “diversion almost certainly occurs at every institution that handles controlled substances, and the rate of discovery of diversion events has increased steadily over the past decade. “ And while most facilities have certain protocols in place, there is no formal set of rules to govern all, so there remains lots of gray areas which allow employees to slip through the cracks.
Read more