Survivor Stories Blog
May is Viral Hepatitis Month

May is Viral Hepatitis Month
Here are some facts to support Viral Hepatitis Month:
- CDC released new surveillance data on viral hepatitis in the US. It shows that between 2015 and 2016, the number of reported cases of HCV increased by 21.8%. The data confirm that high rates of injection drug use, lack of access to sterile equipment, and the unavailability of testing and treatment for lower-income and incarcerated people continue to drive a sprawling epidemic of viral hepatitis.
- An estimated 5 million Americans are infected by the hepatitisC virus, which is now the most common cause of death by an infectious disease.
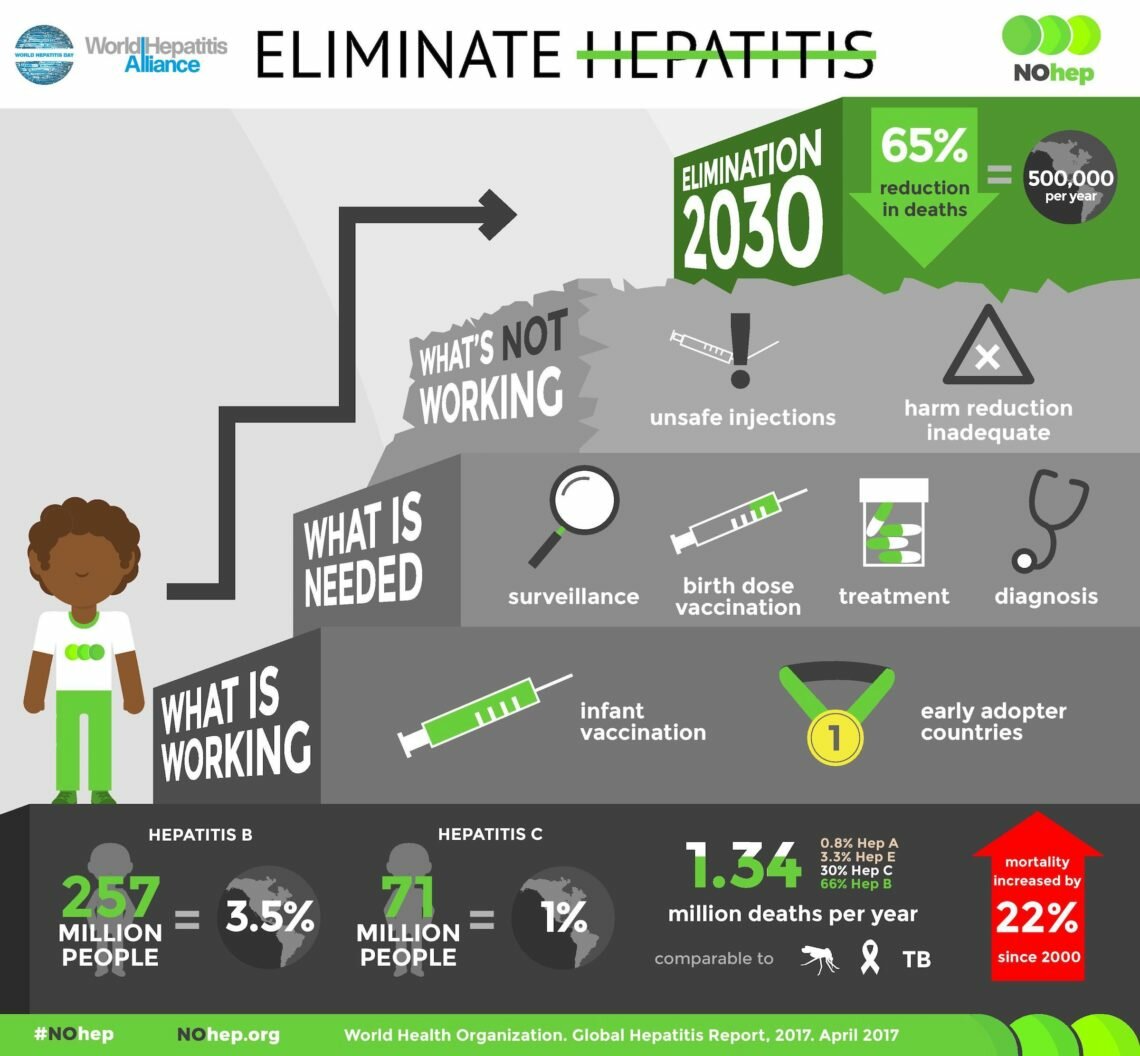
- Globally, there are 1.34M deaths per year from viral hepatitis, which is comparable to the number that dies of malaria, HIV and TB. Mortality has increased by 22% since 2000.
- Unsafe injections have been repeatedly reported from 7 out of 11 countries that carry 50% global burden of hepatitis.
- 30-40% of new hepatitis B&C in developing countries is due to syringe reuse.
World Hepatitis Summit
We were thrilled to participate in the World Hepatitis Summit in Sao Paulo Brazil in November. There were 900 delegates from over 100 countries. It was the launch of NOhep2030. NOhep2030 is a multipronged campaign that encourages prevention, testing, and treatment. A big part of prevention is injection safety. Here is a video recap at this important summit.
NOhep2030 is a campaign to eliminate viral hepatitis by 2030. The campaign is doable because there is now a vaccine for Hepatitis B and cost effective cure for Hepatitis C. My husband and I are thrilled to be part of this effort. As youngsters, our earliest participation in public health was to be part of massive polio vaccination. We think it would be very cool to see within our lifetimes the elimination of two deadly diseases – polio and viral hepatitis.
We will need everyone’s participation to eliminate viral hepatitis. I urge you to visit NOhep.org to see what you can do to help.

Patient Safety Awareness Week

This week is National Patient Safety Awareness week. It is a good time to reflect on patient safety in the United States. We can all work together to improve awarenss of the need for improved patient safety.
There are many estimates about how many people are harmed through preventable medical error each year. Estimates suggest that about 100,000 to 440,000 people die per year from preventable medical error each year. Many more sustain harm that was significant but not fatal.
One life destroyed by medical error is one too many. But these numbers suggest that annually hundreds of thousands of people have their lives destroyed by preventable medical error. These numbers represent real lives of real people. We are all patients. We are all at risk for suffering caused by healthcare. We must take action to save ourselves and those we love from harm sustained through healthcare.
In my home state, we have the means to examine adverse events and educate for prevention through the Nebraska Coalition fo Patient Safety (NCPS). NCPS collects voluntary reports of suspected medical error from medical facilities. It aggregates the data to develop feedback, training and education about causes of medical error and shares the learning with member facilities. Members receive feedback on events, root cause analysis support, information and evidence-based best practices, and patient safety culture development.
However, when the NCPS was established in 2005, a consistent vehicle for funding was not established. The Coalition depends upon voluntary membership dues; this limited and uncertain budget hampers NCPS reach and effectiveness.
Last month, I jumped at an opportunity to increase patient safety in Nebraska by working on legislation to create consistent funding for NCPS. A bill to provide additional fees to some licensed healthcare providers to create the Patient Safety Cash Fund was introduced as LB1127. If passed, $10 will be collected per year from licensed physicians, nurses, pharmacists, occupational and physical therapists to create the Patient Safety Cash Fund. This fund would go directly to the Nebraska Coalition for Patient Safety.
If LB 1127 is enacted, the Coalition will:
- expand their work from hospitals only to the continuum of care;
- engage all healthcare stakeholders, regardless of their position on the current bill, to conduct a patient safety needs assessment, develop a strategy to address cross-cutting priority needs, and then evaluate the effectiveness of our efforts;
- hire additional staff with knowledge and skills in clinical care, informatics, human factors, and organizational culture to receive the increased volume of reports and aggregate and analyze them (while reserving funds for office space, computers, software, and web support);
- implement a communication plan to provide feedback to healthcare professionals and the public using aggregate data to describe the patient safety hazards we identify and the resources needed to address them; and
- expand efforts to ensure all healthcare professionals have the language and tools needed to advocate for patients.
In summary, LB 1127 has the power to engage all healthcare professionals in Nebraska in our most important priority…keeping patients safe while receiving care that is intended to help them.
I’m pleased to report that the Health and Human Services Committee held an executive session and voted to advance patient safety bill LB 1127 to General File! We will continue to work with other committed organizations like the Nebraska Medical Association and the Nebraska Hospital Association to pass the bill and increase patient safety!
Celebrating Infection Preventionists!

This week we celebrate Infection Preventionists during International Infection Prevention Week.
We want to take a moment to thank the committed professionals who keep healthcare safe.
We admire their selfless dedication to important details in medical settings. Their vigilance and leadership is the difference between safe outcomes for patients, and disaster.
Here is an explanation of the work that Infection Preventionists do, taken from the website of the Association of Professionals in Infection Prevention:
The Association for Professionals in Infection Control and Epidemiology (APIC) is the leading professional association for infection preventionists (IPs) with more than 15,000 members. Our mission is to create a safer world through the prevention of infection. This is achieved by the provision of better care to promote better health at a lower cost.
Most APIC members are nurses, physicians, public health professionals, epidemiologists, microbiologists, or medical technologists who:
- Collect, analyze, and interpret health data in order to track infection trends, plan appropriate interventions, measure success, and report relevant data to public health agencies.
- Establish scientifically based infection prevention practices and collaborate with the healthcare team to assure implementation.
- Work to prevent healthcare-associated infections (HAIs) in healthcare facilities by isolating sources of infections and limiting their transmission.
- Educate healthcare personnel and the public about infectious diseases and how to limit their spread.
Many IPs are employed within healthcare institutions and also serve as educators, researchers, consultants, and clinical scientists. The majority of APIC members are affiliated with acute care settings. An increasing number practice in ambulatory and outpatient services where they direct programs that protect patients and personnel from HAIs. Members are also involved in long-term care, home health, and other practice settings where infection prevention and control is an increasing area of responsibility for nurses and other healthcare personnel.
Thank you, Infection Preventionists!

Drug diversion in the Operating Room

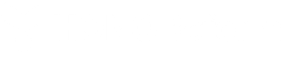
How much harm can a single drug diversion actually cause your facility? All it takes is one stolen or tampered syringe to cause a potential outbreak. Without a watchful eye, entire health care facilities are at risk of exposure.
For example, one diverting surgical technician put 5,900 patients at risk due to their carelessness. Not only did they expose patients to the disease, they also used fentanyl syringes for self-use. It led to 19 confirmed cases of Hepatitis C, and the diverting surgical technician now faces 30 years in prison.
In a separate outbreak instance, another surgical technician potentially exposed 2,900 patients to Hepatitis B, Hepatitis C, and even HIV infection. 2 people tested positive for hepatitis as a result. This surgical technician faces charges of tampering and obtaining fentanyl by deceit.
Lesson learned: all it takes is one irresponsible surgical technician to cause a scare or outbreak. Patient safety is of the utmost importance — keep a watchful eye on any syringes in use. All it takes is one surgical technician to steal a syringe to compromise an entire facility. Check out the infographic below from Diversion Central by Omnicell for more information.
Viral Hepatitis Information from the CDC

The Center for Disease Control and Prevention Division of Viral Hepatitis posts valuable viral hepatitis information. Following is its post commemorating World Hepatitis Day. Visit the CDC’s viral hepatitis webpage for more viral hepatitis information.
Know Hepatitis. Act Now. For World Hepatitis Day, learn more about the different types of viral hepatitis that impact millions worldwide, and what you can do.
Viral hepatitis – a group of infectious diseases known as hepatitis A, B, C, D, and E- affects almost 400 million people worldwide, causing both acute (short-term) and chronic (long-term) liver disease and killing more than 1.4 million people every year. In 2013, viral hepatitis was the seventh leading cause of death worldwide, compared with the tenth in 1990, and caused more deaths than AIDS, tuberculosis, and even road injuries. World Hepatitis Day is July 28th and is an opportunity to highlight the global burden of this disease, CDC’s efforts to combat viral hepatitis around the world, and what actions individuals can take.
What is CDC doing to help combat hepatitis globally?
The vision of CDC is to eliminate viral hepatitis in the United States and worldwide. CDC’s recently released five-year strategic plan[PDF – 17 pages] is organized around four key elements, one of which is “Act globally to prevent, detect, and control viral hepatitis.”
CDC has been re-designated as a Pan American Health Organization/World Health Organization (PAHO/WHO) Collaborating Center for Reference and Research on Viral Hepatitis. These WHO Collaborating Centers work to implement WHO’s Global Hepatitis Strategy priority activities, serving as a reference laboratory, and providing technical assistance for the development of viral hepatitis guidelines and policies.
CDC also assists countries experiencing a high burden of viral hepatitis. In recent years, these countries have included China, Egypt, Georgia, India, Pakistan, and Vietnam. Our international work is helping to reduce the disease burden for travelers and people migrating to the United States, while identifying best practices that may serve as models for other countries, including the United States.
What are the different types of hepatitis viruses occurring around the world?
The five hepatitis viruses – A, B, C, D and E – are distinct; they can have different modes of transmission, affect different populations, and result in different health outcomes. While hepatitis B and hepatitis C cause the greatest global burden of disease, hepatitis A, hepatitis D, and hepatitis E are also global health concerns.
- Hepatitis A is primarily spread when someone who has never been infected with hepatitis A and is not vaccinated, ingests food or water that is contaminated with the feces of an infected person or has direct contact with someone who is infected. Hepatitis A does not cause chronic liver disease and is rarely fatal, but it can cause serious symptoms. Hepatitis A can be prevented through improved sanitation, food safety, and vaccination.
- Hepatitis B is spread through contact with blood or other body fluids of an infected person, including at birth from a mother to her baby and through sexual contact. The hepatitis B virus can cause both acute and chronic infection, ranging in severity from a mild illness lasting a few weeks to a serious, chronic illness. People who are chronically infected can develop liver cirrhosis or even liver cancer. Hepatitis B is most common in sub-Saharan Africa and east Asia, where between 5–10% of the adult population is chronically infected. Rates of chronic hepatitis B are also high in the Amazon region of South America, the southern parts of eastern and central Europe, the Middle East and the Indian subcontinent. Many people with chronic hepatitis B were infected at birth or during early childhood. Getting the hepatitis B vaccine is the most effective way to prevent hepatitis B virus infection. WHO recommends that all infants receive the hepatitis B vaccine as soon as possible after birth. In many parts of the world, widespread infant vaccination programs have led to dramatic declines of new hepatitis B cases.
- Hepatitis C is spread through contact with blood of an infected person. Hepatitis C is common in many countries in the world; in much of Asia and Africa, most infections are caused by unsafe medical injections and other medical procedures. Hepatitis C related to injecting drug use occurs throughout the world; an estimated 67% of people who inject drugs having been infected with the hepatitis C virus. Mother-to-child transmission of hepatitis C is also possible. Hepatitis C, like hepatitis B, can also cause both acute and chronic infections, but most people who get infected develop a chronic infection. A significant number of those who are chronically infected will develop liver cirrhosis or liver cancer. Antiviral medicines can cure approximately 90% of people with hepatitis C, thereby reducing the risk of death from liver cancer and cirrhosis, but access to diagnosis and treatment is low. There is currently no vaccine for hepatitis C but research in this area is ongoing.
- Hepatitis D is passed through contact with infected blood. It only occurs in people who are already infected with the hepatitis B virus. People who are not already infected with hepatitis B can prevent hepatitis D by getting vaccinated against hepatitis B.
- Hepatitis E is spread mainly through contaminated drinking water. Hepatitis E usually clears in 4-6 weeks so there is no specific treatment. However, pregnant women infected with hepatitis E are at considerable risk of mortality from this infection. Hepatitis E is found worldwide, but the number of infections is highest in East and South Asia. Improved sanitation and food safety can help prevent new cases of hepatitis E. A vaccine to prevent hepatitis E has been developed and is licensed in China, but is not yet available elsewhere.
Do you need to be vaccinated and/or tested for hepatitis?
CDC and DVH are continuing to lay the foundation for the elimination of viral hepatitis as a public health threat, both domestically and abroad. Hepatitis A, hepatitis B, and hepatitis C are the most common types of viral hepatitis in the United States. To see if you need to be tested and/or vaccinated for hepatitis A, B, or C, take CDC’s online Hepatitis Risk Assessment, which is based on U.S. recommendations.
More Information
- World Hepatitis Day resource page
- DVH World Hepatitis Day Resources
- World Health Organization
- World Hepatitis Alliance
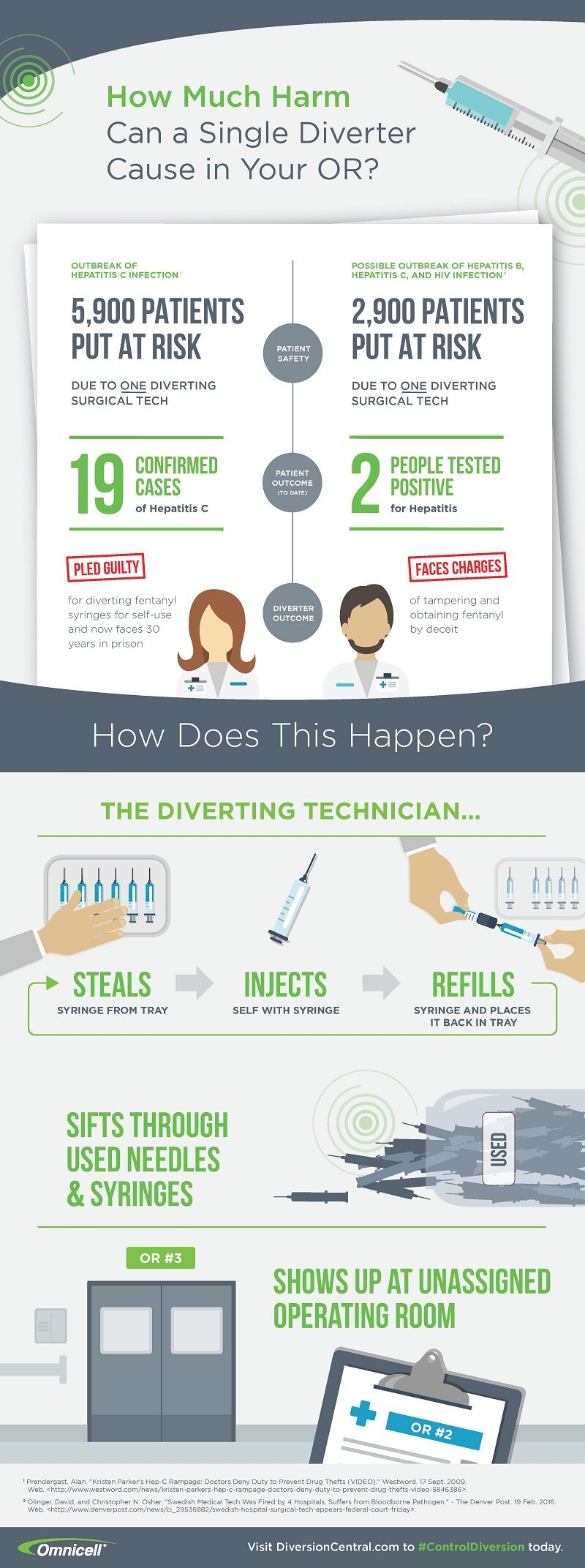
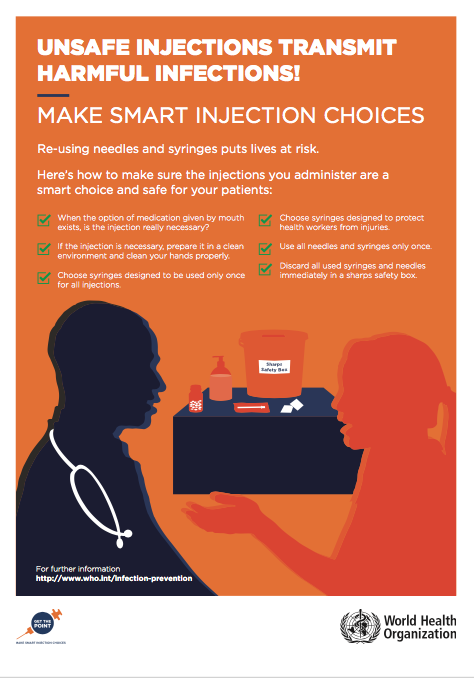
Unsafe Injections transmit Infections!

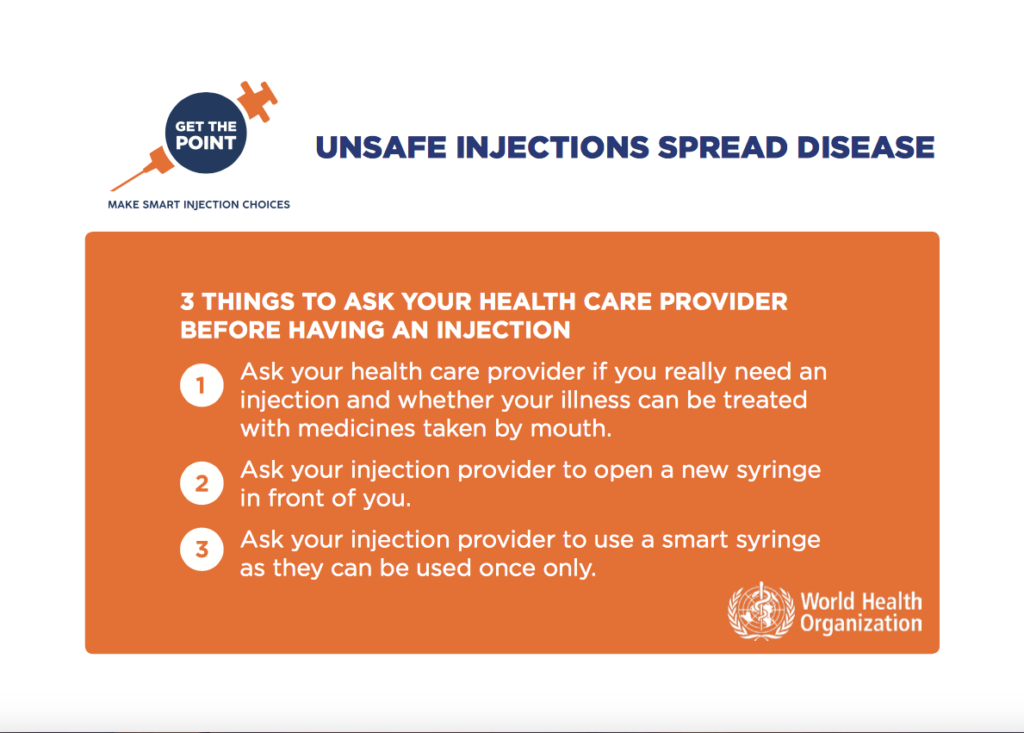
As we commemorate World Hepatitis Day, we remember that unsafe infections transmit infections. We are grateful to the World Health Organization for its efforts in preventing viral hepatitis globally. Many cases of viral hepatitis are transmitted by unsafe injections. Following is a poster to guide healthcare providers in administering safe injections.
Make Smart Injection Choices

The World Health Organization reminds us that we need to make smart injection choices. Following are the questions that the WHO suggests we ask our healthcare provider before we receive an injection to help us make smart injection choices. Unsafe injections spread diseases such as viral hepatitis. When we communicate with our healthcare providers we make good decisions and healthcare improves.
Unsafe injections can transmit hepatitis
World Hepatitis Day is later this week, but it is not too early to prepare! Today we share information about unsafe injections which can transmit hepatitis.
Today we are sharing a poster prepared by the World Health Organization on making smart injection choices. Do you know how to make sure medical injections are safe for you and your family?
Please take a look at the poster and share with your networks. Watch for more information this week. But most importantly, do what you can to make sure injections don’t transmit hepatitis!
World Hepatitis Day is July 28

World Hepatitis Day is later this week, but it is not too early to prepare! This week we will be sharing information about these deadly diseases and how to prevent them.
Today we are sharing an infographic prepared by the World Hepatitis Alliance on the number of cases, causes and cures of Hepatitis B and C. Did you know that the mortality rate has increased by 22% since 2000?
Please take a look at the infographic and share with your networks. Watch for more information this week. But most importantly, do what you can to eliminate hepatitis!
Drug diversion exposes patients to disease

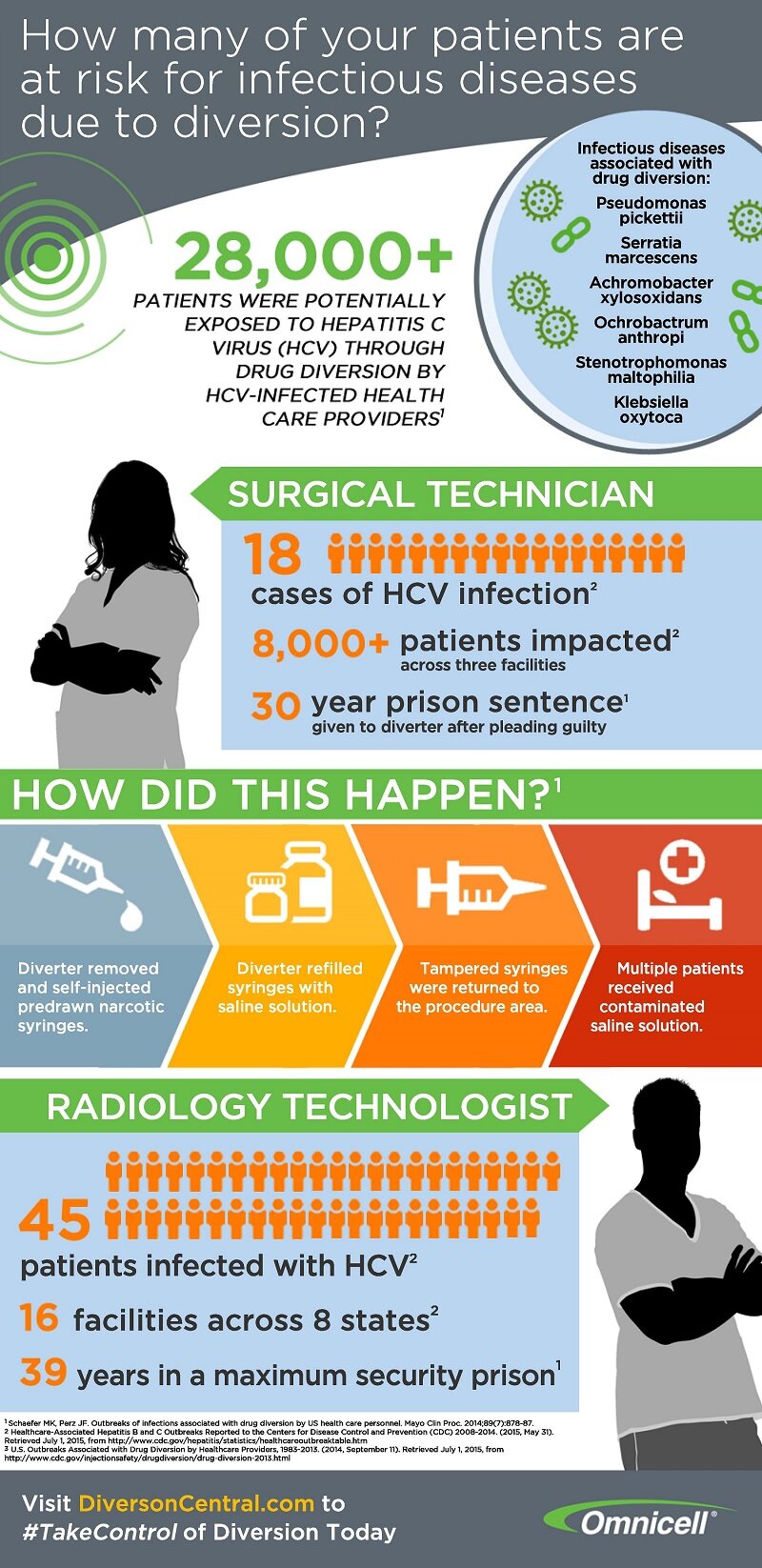
These days, we see drug diversion incidents appear in the news at an increasing rate. 28,000+ patients were potentially exposed to Hepatitis C Virus (HCV) through drug diversion. All of this was due to the carelessness of HCV-infected health care providers.
While its tempting to dismiss as a rare happening, this high exposure rate can happen anytime without proper precautions. For example, one surgical technician caused 18 cases of HCV infection with more than 8000 total patients impacted across three facilities. This single event resulted in a 30-year prison sentence for the diverter.
Although these numbers are staggering, it is easy to lose sight of the fact that these numbers represent real people. These people’s lives were devastated because a healthcare provider tampered with needles, syringes or medication vials to get ‘high’. These people could have been your child, your spouse, your mother. If you access healthcare, it could happen to you. The irony is that these people acessed healthcare seeking better health, but in the process, were exposed to a deadlly disease. And the situation is completely preventable with procedures and policies in place that are designed to prevent drug diversion.
Drug diversions can spread more than HCV. Other infections diseases associated with drug diversion include: pseudomonas pickettii, serratia marcescens, achromobacter xylosoxidans, ochrobactrum anthropi, stenotrophomonas maltophilia, and klebsiella oxytoca. It’s imperative to educate yourself on these diseases and how they can spread from drug diversion.
Patient safety is of the utmost importance, so arm yourself with knowledge of how to prevent, address, and handle drug diversions. Ensure all of your syringes and saline solution are not compromised or tampered with. Check out the infographic below from Diversion Central by Omnicell for more information.